The looming threat: Haemophilus influenzae Type b makes a comeback amid declining vaccination rates

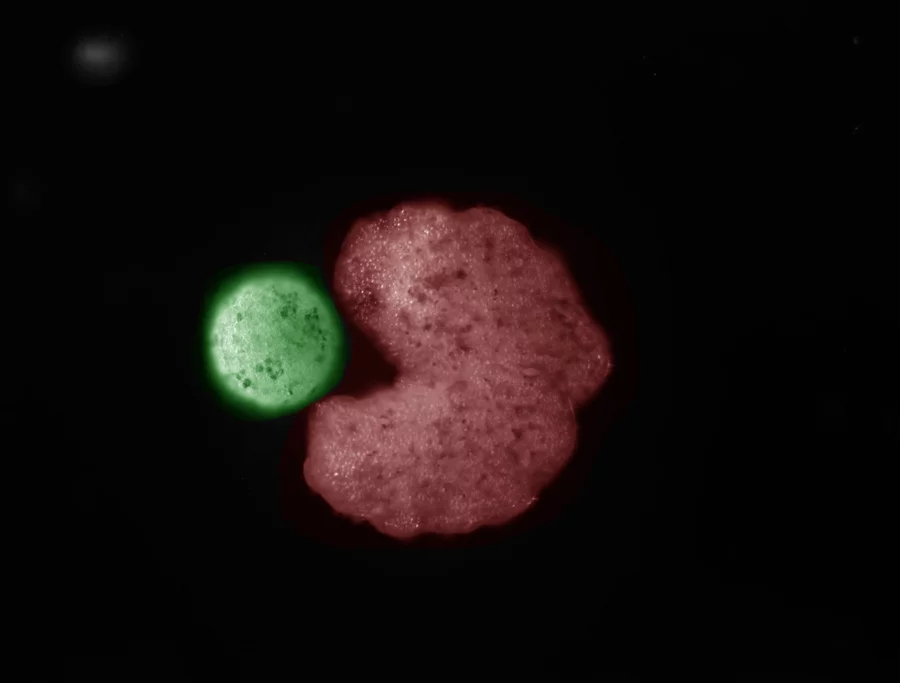
The Haemophilus influenzae type b (Hib) vaccine has been a cornerstone of modern medicine. Introduced in the late 1980s, it transformed a once-deadly bacterium into a rare threat in developed nations.
Hib, which can cause severe illnesses like meningitis, pneumonia, and epiglottitis, primarily targets children under 5.
Before the vaccine, it was a leading cause of bacterial meningitis in the U.S., with thousands of cases annually.
Today, fewer than 50 cases occur each year, a testament to the vaccine’s efficacy. Globally, Hib meningitis cases plummeted by nearly 90% between 2000 and 2015, thanks to widespread vaccination.
Yet, this progress is fragile. Recent incidents in the U.S. and Europe signal that Hib could stage a comeback.
Declining vaccination rates, driven by misinformation and vaccine hesitancy, threaten to unravel decades of success.
Public health experts warn that without action, Hib and other preventable diseases could surge, putting vulnerable children at risk.
Alarming Cases in New York
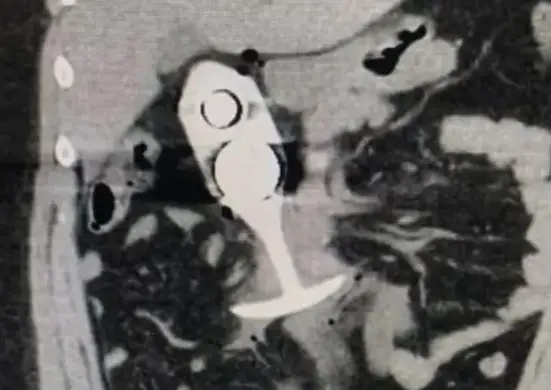
In New York, two unvaccinated infants were diagnosed with Hib meningitis in 2022 and 2023, raising red flags.
The first case involved a 3-month-old girl who presented with fever, lethargy, and seizures.
She required intensive care, surgical drainage for subdural empyemas, and ongoing antiepileptic medication.
The second case, a 5-month-old boy born prematurely, developed septic shock and cerebral edema.
He needed intubation and suffered severe neurologic injury, requiring long-term rehabilitation on ventilation.
Genetic analysis showed the bacterial isolates were closely related, suggesting community transmission.
These cases are particularly concerning given vaccination trends in New York. In 2021, less than 65% of children received their primary Hib vaccination series by 7 months, though coverage reached about 90% by 13 months.
The target for Hib control is at least 70% coverage, given its basic reproductive rate of 3.3. Falling short of this threshold leaves communities vulnerable to outbreaks.
Rising Hib Incidence in Europe
Europe is also seeing warning signs. Several countries, including the Netherlands, have reported a small but sustained increase in invasive Hib disease, particularly among young children.
In the Netherlands, Hib incidence rose from less than 0.3 per 100,000 before 2019 to 0.39 and 0.33 per 100,000 in 2020 and 2021, respectively.
About 40% of cases occurred in children under 5, with incidences of 3.3 per 100,000 in 2020 and 2.6 per 100,000 in 2021 for the first 8 months.
Several factors may explain this uptick. Changes in vaccination schedules—from a 3+1 to a 2+1 regimen—resulted in lower antibody levels in some children.
Additionally, a new vaccine product introduced in 2019 showed slightly reduced immune response compared to previous formulations.
Behavioral factors, such as higher transmission in communities with lower vaccination uptake, like the Netherlands’ Bible Belt, also played a role.
Despite high vaccine effectiveness (91-97%), these changes highlight the need for vigilant monitoring.
The Global Vaccination Landscape
Globally, Hib vaccination coverage remains strong but uneven. By the end of 2023, 77% of children worldwide received three doses of the Hib vaccine, according to the World Health Organization.
However, regional disparities persist, and even in developed nations, coverage is slipping. In the U.S., kindergarten vaccination rates for vaccines like MMR have fallen below the 95% threshold needed for herd immunity.
In 2023-24, 39 states reported rates below this level, up from 28 states in 2019-20.
This decline is not limited to Hib or MMR. A broader trend of falling childhood immunization rates threatens multiple vaccine-preventable diseases.
A study published in JAMA predicts that if current trends continue, millions of infections could occur over the next 25 years.
For measles, the study estimates 851,300 cases, 2,550 deaths, and 170,200 hospitalizations.
While Hib-specific projections are less common, the same principles apply: lower vaccination rates increase the risk of resurgence.
Vaccine Hesitancy: A Growing Threat
Vaccine hesitancy is a key driver of declining immunization rates. Fueled by misinformation on social media and false claims by public figures, hesitancy has grown significantly.
A Gallup survey found that the percentage of U.S. parents who view childhood vaccinations as “very” or “extremely important” dropped from 94% in 2001 to 69% in 2024.
Surveys from 2021-2023 show declining confidence in vaccine safety, with some parents believing vaccines contain toxins or cause disease.
This hesitancy has tangible consequences. The share of kindergarten children with nonmedical exemptions has risen, contributing to outbreaks of vaccine-preventable diseases.
In 2024, the U.S. saw 16 measles outbreaks, compared to 4 in 2023, with 40% of cases requiring hospitalization.
While measles is more contagious than Hib, the trend underscores the broader risk to diseases like Hib if vaccination rates continue to fall.
| Region & Year | Hib Incidence, Vaccination Coverage & Key Notes |
|---|---|
| New York, USA (2021) | Incidence: <50 cases annually Coverage: <65% by 7 months, ~90% by 13 months Notes: Two severe cases in unvaccinated infants, 2022-2023 (CDC Emerging Infectious Diseases) |
| Netherlands (2020-2021) | Incidence: 0.39 per 100,000 (2020), 0.33 per 100,000 (2021) Coverage: High, but schedule changes impacted immunity Notes: 40% of cases in children under 5 (PMC Netherlands Study) |
| Global (2023) | Incidence: Not specified Coverage: 77% with 3 doses Notes: Uneven coverage increases outbreak risk (WHO Immunization Coverage) |
The Consequences of Inaction
The potential impact of declining vaccination rates is stark. The JAMA study warns that at current rates, measles could become endemic again within 21 years.
A 25% decline in vaccination coverage could lead to 26.9 million measles cases, nearly 88,000 polio cases, and 80,600 deaths over 25 years.
For Hib, maintaining at least 70% coverage is critical to prevent outbreaks. With some areas already below this threshold, the risk of a Hib resurgence is real.
Hib’s severity adds urgency to the issue. Before vaccines, Hib caused meningitis in thousands of U.S. children annually, with a mortality rate of up to 5% and long-term complications like hearing loss or neurological damage in survivors.
The recent New York cases, with one child facing severe neurologic injury, highlight the stakes.
A Call to Action
The Hib vaccine’s success is a public health milestone, but it is not guaranteed. Recent cases in New York and Europe, coupled with declining vaccination rates and rising hesitancy, serve as a wake-up call.
Public health efforts must focus on countering misinformation, improving vaccine access, and ensuring timely vaccinations.
Community outreach, transparent communication, and collaboration with trusted leaders can rebuild confidence in vaccines.
Parents and caregivers play a critical role. The CDC recommends Hib vaccination for all children under 5, typically in a series of 3 or 4 doses.
For adults, vaccination is generally not needed unless they have specific conditions, like a removed spleen, as natural immunity from childhood exposure or vaccination often persists.
Looking Ahead
The fight against Hib is not over. While the vaccine has made the disease rare, complacency could reverse this progress.
By addressing vaccine hesitancy and ensuring high coverage, we can protect children and communities from the devastating effects of Hib and other preventable diseases.
The choice is clear: act now to maintain the gains of the past, or risk a future where Hib once again threatens young lives.