Georgia abortion law keeps brain-dead pregnant woman on life support, family calls it ‘torture’

Family Endures 90 Days of Trauma as Brain-Dead Daughter Remains on Life Support
In a heart-wrenching case that has ignited debate over Georgia’s stringent abortion laws, 30-year-old Adriana Smith, a mother and nurse from Atlanta, has been kept on life support for over three months after being declared brain dead.
Her family, led by her mother April Newkirk, describes the ordeal as “torture,” emphasizing the lack of control they have over her medical care due to the state’s controversial “heartbeat bill.”
The situation highlights a complex intersection of medical ethics, legal constraints, and family autonomy, drawing attention to the broader implications of Georgia’s abortion policies.

Adriana’s tragic journey began in early February 2025 when, at nine weeks pregnant, she started experiencing severe headaches.
Seeking medical attention, she visited Northside Hospital, where she was prescribed medication and sent home without a CT scan.
The next morning, her boyfriend found her making gurgling noises and gasping for air, a scene he described as terrifying.
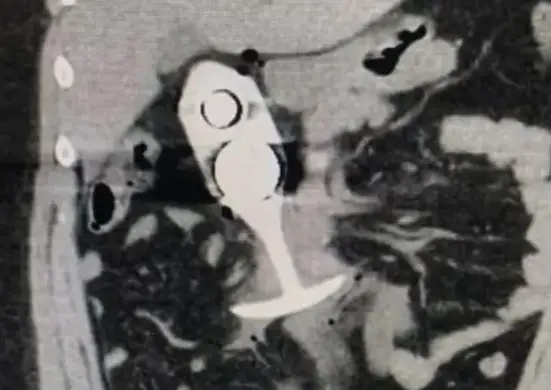
She was rushed to Emory Decatur and then to Emory University Hospital, where a CT scan revealed multiple blood clots in her brain.
Despite medical efforts, she was declared brain dead.
Smith, a registered nurse at Emory University Hospital, was known for her dedication to her patients and her love for her young son.
Her mother shared with 11Alive that the family visits her daily, with her son believing his mother is “just sleeping.”
“I bring him to see her,” Newkirk said. “He thinks she’s just sleeping.”

Georgia’s Heartbeat Law Creates Legal Gray Area
At the core of this case is Georgia’s Living Infants Fairness and Equality (LIFE) Act, also known as the “Heartbeat Bill.”
Signed into law by Governor Brian Kemp in 2019, the law prohibits abortions after six weeks of pregnancy when a fetal heartbeat is detected, with exceptions only for medical emergencies or medically futile pregnancies.
It took effect in July 2022 following the U.S. Supreme Court’s overturning of Roe v. Wade, as reported by Newsweek.
In Adriana’s case, the law has created a legal gray area. Since she is brain dead and no longer considered at risk herself, doctors are legally required to maintain her life support until the fetus reaches viability, estimated at 32 weeks gestation.
Currently, she is 21 weeks pregnant. “She’s been breathing through machines for more than 90 days,” Newkirk told WXIA-TV.
“It’s torture for me. I see my daughter breathing, on a ventilator, but she’s not there. And I’m touching her.”
The law defines a medical emergency as a condition requiring an abortion to prevent the death of the pregnant woman or substantial and irreversible physical impairment.
However, in cases like Adriana’s, where the mother is brain dead, the law’s application becomes ambiguous, leaving families without the ability to make end-of-life decisions.
“I think every woman should have the right to make their own decision,” Newkirk said. “And if not, then their partner or their parents.”

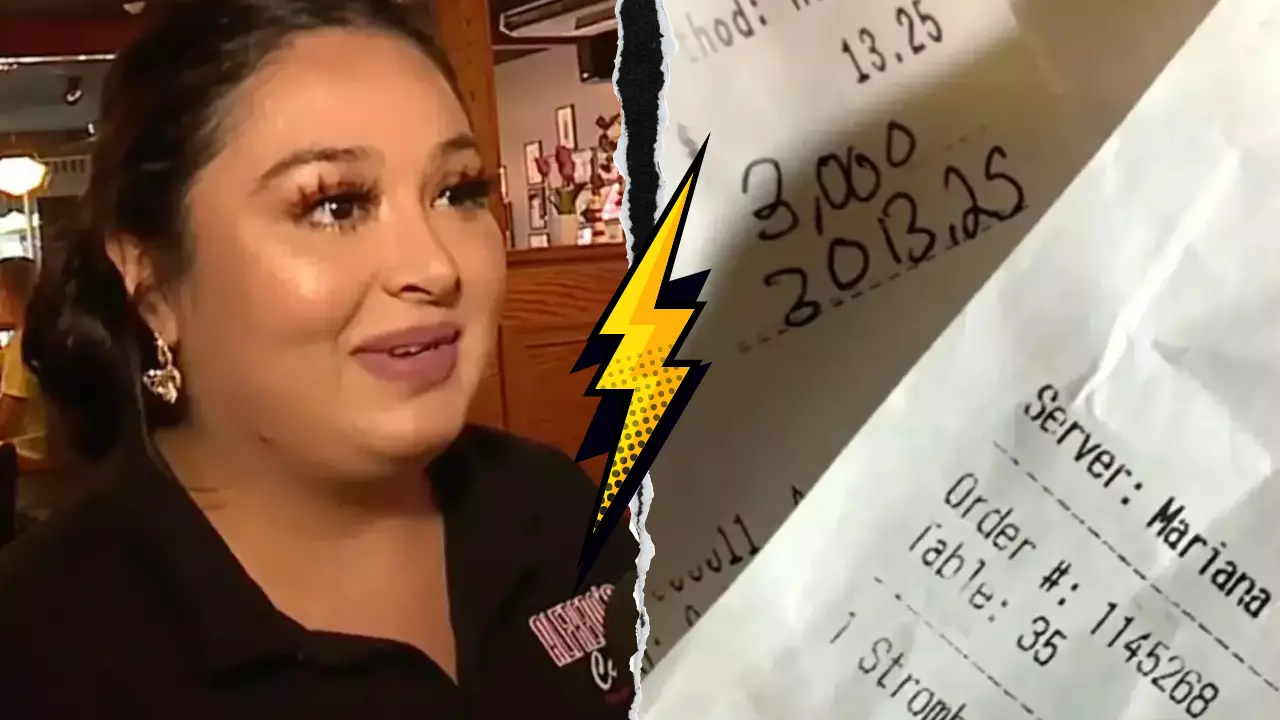
Family Grapples with Emotional and Financial Toll
The emotional toll on the Smith family is profound. Newkirk described the daily visits to see her daughter as “torture.”
“Every day that goes by, it’s more cost, more trauma, more questions,” she told WXIA-TV, referring to the mounting hospital bills and the uncertainty surrounding the baby’s health.
Doctors have informed the family that the baby, a boy, has an unknown amount of fluid on the brain, raising concerns about potential health issues, including blindness, inability to walk, or even survival after birth.
“She’s pregnant with my grandson,” Newkirk said. “But my grandson may be blind, may not be able to walk, may not survive once she has him.”
“This decision should’ve been left to us. Now we’re left wondering what kind of life he’ll have—and we’re going to be the ones raising him.”
The family’s frustration extends to the initial medical care Adriana received.
Newkirk believes the tragedy could have been prevented if Northside Hospital had conducted a CT scan or kept her overnight for observation.
“They gave her some medication, but they didn’t do any tests. No CT scan,” she told 11Alive.
“If they had done that or kept her overnight, they would have caught it. It could have been prevented.”
Adriana has since been moved to Emory Midtown for better obstetric care, where she remains on life support.

Medical and Legal Perspectives Clash
The case underscores the complexities of applying abortion laws to situations involving brain-dead pregnant women.
Emory Healthcare issued a statement: “Emory Healthcare uses consensus from clinical experts, medical literature, and legal guidance to support our providers. Our top priorities continue to be the safety and wellbeing of the patients we serve.”
However, the law’s strict provisions have left little room for family input.
Monica Simpson, executive director of SisterSong, an organization challenging Georgia’s six-week abortion ban, condemned the situation: “Adriana deserved to be trusted by her health care professionals. Her family deserved the right to have decision-making power about her medical decisions.”
“Instead, they have endured over 90 days of re-traumatization, expensive medical costs, and the cruelty of being unable to resolve and move toward healing.”
Governor Brian Kemp, who signed the heartbeat bill into law, has not commented specifically on Adriana’s case.
However, his stance on the law was clear in 2019: “We will not back down. We will always continue to fight for life.”
Broader Implications for Abortion Laws and Medical Ethics
Adriana’s case is not an isolated incident. Georgia’s abortion laws have faced criticism for creating confusion and delaying critical medical care.
ProPublica reported that at least two women in Georgia died after being unable to access legal abortions and timely medical care under similar circumstances.
Kwajelyn Jackson, executive director of the Feminist Women’s Health Center, stated in 2024: “This ban has wreaked havoc on Georgians’ lives, and our patients deserve better… even in light of the deadly consequences we have already witnessed.”
The situation raises profound questions about medical ethics and the role of families in end-of-life decisions.
While the law aims to protect fetal life, it has left families like the Smiths feeling powerless and trapped in a legal and ethical limbo.
Advocacy groups argue for clearer guidelines to ensure families have a say in such complex cases.
| Aspect | Details |
|---|---|
| Patient | Adriana Smith, 30, registered nurse, mother |
| Condition | Declared brain dead, on life support for over 90 days |
| Pregnancy Status | 21 weeks pregnant, target viability at 32 weeks |
| Baby’s Health | Fluid on brain, potential blindness, mobility issues, survival uncertain |
| Legal Constraint | Georgia’s heartbeat law bans abortion after six weeks, no family decision-making power |
| Family Impact | Emotional trauma, financial burden from hospital bills |

A Family’s Heartache and a Call for Change
As Adriana remains on life support, her family continues to advocate for legislative changes to prevent other families from facing similar situations.
With the pregnancy progressing, they await the day when the baby can be delivered, hoping for a healthy outcome while mourning the loss of Adriana.
“Every woman should have the right to make their own decision,” Newkirk reiterated.
“And if not, then their partner or their parents. This should never happen to another family.”
The case has sparked a broader conversation about the need for nuanced laws that balance fetal protection with family autonomy and medical ethics.
As Georgia grapples with these challenges, Adriana’s story serves as a poignant reminder of the human cost of legal ambiguities in healthcare.